Children’s Services Policy
Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Program Services

What is EPSDT?
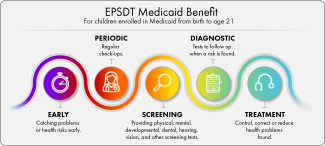
- EPSDT stands for the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Benefit.
- It is a benefit that provides health care services for children under 21 years old who are enrolled in Medicaid. It makes sure that children and adolescents get the services they need, as soon as they need them.
- EPSDT means:
- Early: Catching problems or health risks early.
- Periodic: Regular check-ups.
- Screening: Providing physical, mental, developmental, dental, hearing, vision, and other screening tests.
- Diagnostic: Tests to follow up when a risk is found.
- Treatment: Control, correct or reduce health problems found.
Things You Should Know about the EPSDT Benefit:
- EPSDT covers treatments children and adolescents need to correct or improve birth defects, physical health, and behavioral conditions.
- It’s more extensive than services for adults, emphasizing early care to prevent or treat health issues.
- Quick identification of problems can help avoid increased disabilities. It can also help make sure children and adolescents achieve their future life goals.
- Treatment decisions are based on individual needs.
How to Access EPSDT:
- Speak with your child's treatment team to get them EPSDT services.
- Prior authorization is required for services not normally covered by Medicaid.
Your Rights:
- You have the right to appeal if medical services are denied or not acted upon.
- You can also file a grievance with your managed care organization, if needed.
Preventive Pediatric Schedule
- Click here to view or download the schedule of screenings and assessments recommended at each pediatric well-child visit.
- Click here to view or download the schedule of screenings and assessments recommended at each pediatric oral health visit.
Click below to learn more about related programs and services in Rhode Island.
Katie Beckett is an eligibility category that allows certain children under age 19 who have long term disabilities or complex medical needs to become eligible for Medicaid coverage. Katie Beckett eligibility enables children to be cared for at home instead of in an institution. With Katie Beckett, only the child's income and resources are used to determine eligibility.
A Cedar Family Center provides information and referral about the services and support options available for all children enrolled in Medicaid who have disabilities and special needs.
Early Intervention promotes the growth and development of infants and toddlers who have a developmental disability or delay in one or more areas. Developmental disabilities or delays can affect a child’s speech, physical ability, or social skills. Children referred to the Early Intervention Program receive a comprehensive developmental evaluation to determine if they are eligible.
KIDS CONNECT is a program that provides specialized services at DCYF licensed childcare centers that can help children with special needs participate, play, and learn along with their typically-developing peers. KIDS CONNECT provides an additional staff member in the classroom to support the child with special health care needs.
Personal Assistance Services and Supports (PASS) is a family directed service that can help families of children with special health care needs. PASS is provided in the home or community setting to help improve a child’s ability to do activities of daily life, maintain safety, and/or gain social skills.
Home Based Therapeutic Services (HBTS) are medically necessary, intensive services that can help families of children with moderate to severe behavioral health, developmental or physical disabilities. HBTS is provided to children in the home or community setting.
The Respite Program for Children allow parents or guardians caring for a child with disabilities, to have time off for themselves. To be eligible for the Respite for Children Program, a child must need an institutional level of care that can best be described as the type of care typically provided in a hospital, nursing home or Intermediate Care Facility for the Mentally Retarded (ICF/MR).
Parents / guardians are required to find their own respite worker. Assistance is available from certified Respite agencies
The Rhode Island Medicaid Programs for Children with Special Healthcare Needs contains an account of services and supports available to Medicaid eligible children and their families (Fee for Service Medicaid, Neighborhood Health Plan of RI, Tufts Health Plan , and UnitedHealthcare Community Plan).
RI Medicaid Programs for Children (5/2024)
- For 18-21 in DCYF
- Adolescent Healthcare Transition Program
- Adolescent Transition for People with Special Health Care Needs
- Independent Living Program
- Sherlock Plan Guide
- The Sherlock Plan: Regulations
- Rhode Island Parent Information Network(RIPIN), Transition to Adulthood
- Applying for Supplemental Security Income (SSI) for a child